
Sherry passed away this afternoon, naturally and peacefully in her sleep.
She loved her community and we know how grateful she was to every one of her friends on here for the genuine love and support she’s received over the years.
We (her family) are processing, but will share details about her celebration of life when we’ve worked it out.
Sherry’s Slideshow:
Cushing’s Help message board member sherryc presented this PowerPoint at Pioneer Pacific College. It took a lot of work with her failing memory but she did It! She wanted to get the word out about Cushing’s and her journey with this awful disease.
She says that it took a lot of work with her failing memory but she did It! She wanted to get the word out about Cushing’s and her journey with this awful disease.
Sherry’s bio:
I have been very ill for many years now, since 1999 that I know of. But it had always come and gone, until 2004 when it decided to stay. At first it was a mystery as to what was wrong. I was seeing a psychiatrist that felt very strong that what I was dealing with was endocrine related. He mentioned a few things that it could be and one was Cushing’s, so I looked it up on the internet and sure enough I had many of the symptoms of Cushing’s disease, moon face, buffalo hump, weight gain, big round belly, red face, very ruddy complexion, acne, nausea, depression, fatigue, hirsutism, depression, anxiety, hypertension, unusual bruising, and highs and lows of energy.
I found this support group on the internet at Cushings-help.com and they helped me find Dr.William Ludlam at OHSU. He told me I had a suddle case of Cushing’s and had a pituitary tumor on the right side displacing the pituitary to the left. Although Dr.Ludlam originally saw tumors on both sides, I had a pituitary tumor that seemed to be cyclic. When it turned on I had major Cortisol energy, when it turned off I got very achy, nausea, and very tired. In March of 2006 I was officially diagnosed after 1 long year of testing, and went on to have my first unsuccessful Transphenoidal pituitary surgery 3/23/2006 with Dr. Johnny Delashaw at OHSU. I had a second unsuccessful pituitary surgery 10/12/06 and finally a BLA 11/7/06.
I am now cured of Cushing’s disease 2 1/2 years out from my BLA and I am still very sick, I traded Cushing’s disease for Addison’s disease, and my body does not like it. Cushing’s did a lot more damage than ever thought; I have permanent nerve damage to my lower back, damage to soft tissues throughout my body, Diabetes, High lipids, Fatty liver, I have no usable veins, I have permanent port-a-cath in now so they can access my veins for blood draws and any IV stuff I may need in emergency’s. I had my period for 1 year straight so I had a full hysterectomy 8/20/08. I am permanently panhypopituitary now, no working hormones any more. I am on all replacement hormones, except DDAVP. I ended up with a new doctor that gave me a severe case of steroid induced Cushing’s. I am still dealing with this aftermath; the details are in my timeline. My timeline will update you as to where I am at now. I will try to keep the timeline updated so you know where I am at as far as getting better.
Please don’t let this scare you, most people are cured and go on to live lives as best they can, and a lot of people are doing very well. Towards the end of my Cushing’s I went full blown, Dr.Ludlam told me this was a progressive disease and in me this was the case.
So if you believe you have Cushing’s, get to a specialist that knows Cushing’s disease, don’t waste time on doctors that do not know the disease, it is so worth it in the end to get to the right doctor. This disease is one of the hardest endocrine diseases to diagnose. Cushings_help.com/ founder MaryO has been a lifesaver for me and still is, I have met people from all over the country, over the years I have made many friends that have, had or are still in the diagnostic phase.
I live in a small town of around 10,000 people and I hear all the time, oh I know so and so that had or has a pituitary tumor. What I am finding out is there are a lot of people in this town that have this disease, it is suppose to be rare, one in a million, my next goal is to get my story out and have local people contact me, then start a support group. Maybe get some accurate numbers of actual pituitary/brain tumors and find out why this is happening in this small town. It will be a big adventure but if it saved even one life it will be worth it. I know of 3 definite pituitary Cushing’s cases so far.
My Timeline of illness to diagnosis
3rd pregnancy 1994 pre-term labor again, stopped, gestational diabetes, son born 3 weeks early and I got toxemia after my son was born, was told this is very rare. I should have known RARE would be a word I would hear a lot in my future.
1995-Left breast discharge, surgical biopsy done, lump removal of marble size, this should have signaled a full hormonal work-up, but didn’t. No cancer.
1997-1999 Depression and severe anxiety with panic attacks…Diagnosis of Fibromyalgia. Weight 130#
1999- First occurrence of unknown mystery illness. Hypertension, fatigue, flushing, swelling of face, hives, and much more that lasted several months. Sick on and off with mystery illness. Tumor was turning on and off.
April 1999-2004-Severe nausea and vomiting, extreme fatigue, weight gain of 50# in about 1 years time, headaches, dizziness, hypertension, tachycardia, muscle and bone pain, malor rash, other rashes, IBS, occasional unexplained low grade fevers, anxiety and depression much worse, increased hirsutism, almost constant mouth sores, memory loss, cognitive difficulties, loss of coordination, syncope, excessive energy spurts, insomnia.
**Off work for 3 months April-June due to symptoms…Saw PCP, Gastroenterologist, Rheumatologist and Cardiologist… diagnosis Peptic ulcer/Chronis Gastritis and Chronic pain Syndrome and Tachycardia/Hypertension. Abdominal/Pelvic Cat scan done and fatty liver noted. High Cholesterol and Triglycerides discovered.
Nov-2004 My Psychiatrist was the first to mention Cushing’s or a Pheochromocytoma; he felt all my symptoms where due to endocrinology. He did not want to see me again until I was seen at OHSU. I have never seen him again due to insurance change. I really need to thank him.
Dec-2004 10# weight gain in 1 week with severe abdominal distention….another Cat scan done, lymph nodes around vena cava where enlarged.
Jan-2005 Went to OHSU for diagnosis….First saw an endocrinologist that was not experienced with Cushing’s, she ordered 1 UFC and 2 midnight saliva tests, and told me to test when I felt my worst; Tests where low so she felt my symptoms where not due to my endocrine system. Boy was she wrong. I needed to test when I felt good, or high.
Feb-2005 Went to the Pituitary Unit at OHSU and saw Dr.Ludlam, he believed that I had Cushing’s but we needed to prove it. MRI saw adenoma on right side displacing pituitary to the left. He originally thought he saw tumors on both sides, he was right. Lot’s of testing done. Testing did not prove it yet. Dr believes I am Cyclic. It took 1 year for diagnoses from Dr.Ludlam.
April-2005 Peripheral vision test done by local optometrist, showed some peripheral loss in left eye.
May 2005-Lot’s more Cushing’s testing, PICC line in all month. Major dizziness, passed out and fell this month. Diagnosed with Type 2 Diabetes but cannot treat due to extreme highs and lows, trying to control glucose with diet. I have very high and low Cortisol days. I am very cyclic at this point.
June/July 2005-Three TIA like event’s… left sided weakness and numbness. Saw Neurologist that sent me to Neurologist at OHSU. Found three new white matter lesions seen on my brain MRI. Unknown cause. 5 in all now.
August 2005-Had to leave my beloved job teaching Medical Assistants due to symptoms. I had one more TIA like event.
Sep-2005 Neurologist at OHSU ran several tests and came to the conclusion that if in fact we could prove Cushing’s, all of my symptoms where due to this disease. I stopped all medications by choice.
Nov-2005 I went back for extensive testing at OHSU with Dr.Ludlam and sure enough the numbers started proving my case. Very high midnight serum Cortisol’s among other high tests.
Jan/Feb 2006-PICC line in and extensive Cushing’s testing done with CSS in Feb. CSS showed left sided gradient strongly. Cortisol numbers have proven my case, finally…. I had a midnight serum Cortisol of 34.1, the Midnight Salivaries, Midnight Serum Cortisol, UFC’s and CSS all positive for Cushing’s disease.
March 23, 2006 I finally had Pituitary surgery at OHSU, they found the tumor on the left side bigger than originally though and removed the whole left half of my Pituitary gland. I was in the hospital for 6-days due to complications of Diabetes Insipitus and Adrenal Insuffiency.
April-2006 Seen in the ER 3 times. Hospitalized for 4 days again due to complications, Blood cultures showed infection. I am on very high doses of Hydrocortisone and also taking DDAVP for the Diabetes Insipitus.
April 2006- I am finally getting better somewhat…..This has been one heck of a roller coaster ride. I am now on Hydrocortisone 40/40/30. I am told we won’t know if I am cured for 3-6 month’s.
June 5, 2006- Off Hydrocortisone stimulated my Cortisol to 24 on the ACTH stim test.
August, 2006- Not cured, testing again!!! I had that gut feeling when I woke from the first surgery. I just knew…
October 12, 2006- Second Pituitary surgery, more tumor on right side, most of my pituitary gland removed. Surgery unsuccessful, still have Cushing’s disease.
November 7, 2006- BLA …soon to be cured of Cushing’s.
Dec 2006/Jan 2007- Very sick due to another blood infection. Lot’s of adrenal crises due to infections. 3 blood infections to date.
November 2008- 2 years out from my BLA and I am still very sick, I traded Cushing’s disease for Addison’s disease, and my body does not like it. Towards the end of my Cushing’s I went full blown, Dr.Ludlam told me this was a progressive disease and in me this was the case. Cushing’s did a lot more damage than ever thought; I have permanent nerve damage to my lower back requiring permanent narcotic pain relief through a pain center, damage to soft tissues throughout my body, diabetes, high lipids, fatty liver (NASH), Osteopenia, I have no usable veins, they are destroyed due to the high Cortisol, I have permanent port-a-cath in now so they can access my veins for blood draws and any IV stuff I may need, I had my period for 1 year straight because of lack of appropriate hormones after my surgeries so I had a full hysterectomy 8/20/08. I am permanently panhypopituitary now, no working pituitary hormones any more at all. I must replace all pituitary hormones, except DDAVP. Please don’t let this scare you, most people are cured and go on to live lives as best they can, and a lot of people are doing very well.
June 21, 2009-Since writing in November I sat on the couch in severe AI until around September when I was put with a doctor that has been seeing Cushing’s patients for 38 years, he put me a on a very high dose of Dexamthasone and Florinef and forgot about me, he ended up with cancer and is no longer seeing patients. In the meantime, I got severe steroid induced Cushing’s and have had severe complications from it. I started falling from atrophied muscles and broke both hips, I ended up in a wheelchair, which I am happy to say I am out of now, had to have surgery on my left hip to pin it, it is still not healing, I am having absorption issues with calcium, iron, vitamins, minerals and meds. So I have to do my DEX by injections. We are now trying to find out why I am having absorption issues. I have a new endo at OHSU Dr.V and he is wonderful. He has brought my steroids down to a safe level and did it slow. He really seems to know his stuff as far as after care. I do not think he does the diagnosis process for Cushing’s. I would definitely go back to Dr.Ludlam if I had to go through it again. But I know there are many other great Cushing’s experts out there, this was just my experience. I know I will get better, but it may be a while. I am still at home handicapped, can barely go to the grocery store and I do not drive as I am on a high dose of Morphine. My goal is to get my pain under a 5 and be able to drive myself around. That is a good goal for now. Then on to finding out why my small town has so many tumors and starting a support group. I just need to get to a point where I feel I can be a good advocate for Cushing’s and right now I can’t. But that is the goal.
Nov 16, 2009
I am still not well, I have broken my ankle, have no idea how, woke up one morning and it was broken. I am almost down to my 1/2 mg of DEX and am happy about that. had 2 surgeries in Sep and Oct on both elbows for ulnar nerve decompression. The first surgery got infected and a week later I had sepsis, which they think I had a small bowel preferation that healed itself. I was ambulanced up to OHSU and was in AI. It was a very rare bowel bacteria running through my blood stream, I was very sick. I just want to get well, but for some reason I am going through one thing after another. I am praying that 2010 will be my year of healing and I will have a good quaility of life then.That is what I am counting on.
UPDATE January 23, 2016
2016: wow has the past few years have been a roller coaster. I don’t know dates because I’m having memory issues at 47 years old.
I have had 5 port-a-caths. I kept getting sepsis and every time they would take me to surgery and remove my port. Then place another when I was better. I have no veins that work. So I received IV port fluids 2-3x a week. I just recently had sepsis, when I get it I have a 50/50 % chance of survival. They removed my port and did not place another. So no more fluids which was for Pots. I had labs done through my port every 2 weeks. Now everything stopped. I am producing small amounts of cortisol. After a BLA.
Intermittently. I am just now starting to feel good for 2 weeks now. I have started the exercise program called T-Tapp. I love it. No jumping or hard moves. 15 min and that’s it. I am a grandma of 2 and one due any day.
So for now I hope I’m on the road to recovery at least the best I can.
HOME | Sitemap | Abbreviations | Adrenal Crisis! | Glossary | Forums | Bios | Add Your Bio | Add Your Doctor | MemberMap | CushieWiki
Like this:
Like Loading...









 What do you do for self care? Please tell me in the comments.
What do you do for self care? Please tell me in the comments.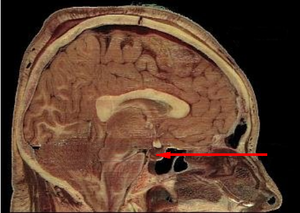


Recent Comments